MOUNT SINAI – New York – A new study by researchers at the Icahn School of Medicine at Mount Sinai reveals that artificial intelligence (AI) has the potential to predict which critically ill patients on ventilators are at risk of underfeeding. This capability could enable clinicians to intervene sooner, thereby improving patient care. The study’s findings were published in the online issue of Nature Communications on December 17.
The researchers highlight that the first week of ventilation is crucial for providing adequate nutrition, as patients’ needs can change rapidly during this time. “Too many patients on ventilators in the intensive care unit (ICU) don’t get the nutrition they need during the critical first week,” said co-senior corresponding author Ankit Sakhuja, MBBS, MS, Associate Professor of Artificial Intelligence and Human Health, and Medicine (Data-Driven and Digital Medicine). “We wanted to explore a simple, timely way to identify who is most at risk of being underfed so that clinicians could intervene earlier.”
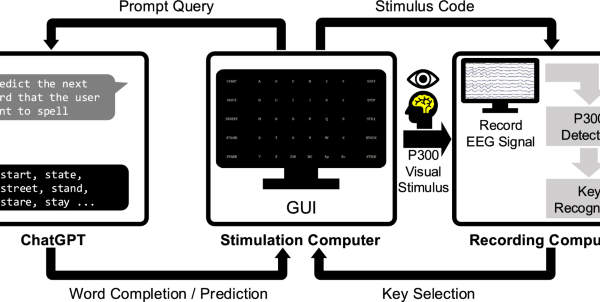
The study’s research team developed an AI tool named NutriSight, which analyzes routine ICU data—including vital signs, lab results, medications, and feeding information—to predict, in advance, which patients may be underfed on days three through seven of ventilation. Using large deidentified ICU datasets from Europe and the United States, the model updates its predictions every four hours as patient conditions evolve.
The findings from the study reveal several significant insights that could enhance patient care. Notably, underfeeding is prevalent early in ICU treatment, with approximately 41 percent to 53 percent of patients identified as underfed by day three, and about 25 percent to 35 percent remaining underfed by day seven. The model is dynamic and interpretable, allowing clinicians to see which factors—such as blood pressure, sodium levels, or sedation—impact the risk of underfeeding.
According to the investigators, NutriSight is not designed to replace clinicians but rather to function as an early-warning system that can guide timely nutritional interventions. The next steps for the research team include conducting prospective multi-site trials to assess whether acting on these predictions leads to improved patient outcomes, integrating the model into electronic health records, and expanding its application to more personalized nutrition targets.
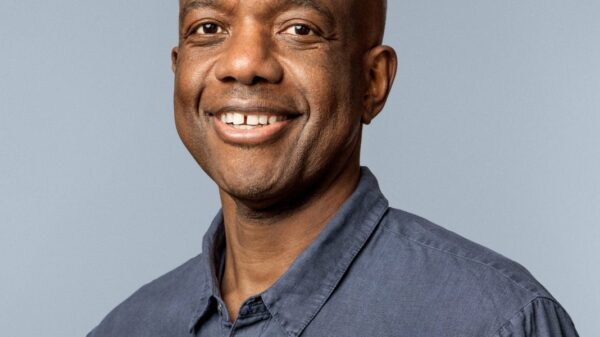
The significance of this study, according to co-senior author Girish N. Nadkarni, MD, MPH, Chair of the Windreich Department of Artificial Intelligence and Human Health, is that it marks a pivotal point in identifying patients at risk of underfeeding early in their ICU stays. “It represents an important step towards giving clinicians better information to make decisions about nutrition,” Nadkarni stated. “Ultimately, the goal is to provide the right amount of nutrition to the right patient at the right time, which could enhance recovery and outcomes for critically ill patients.”
This research was supported by a grant from the National Institutes of Health (NIH), specifically grant K08DK131286. The full study can be accessed in Nature Communications for additional details on potential conflicts of interest.
As AI continues to make inroads into healthcare, tools like NutriSight may revolutionize how clinicians approach nutrition management for critically ill patients, paving the way for more customized care strategies. For further information on Mount Sinai‘s advances in artificial intelligence, visit their official website.
See also LIBA’s Rev. Dr. Arun: Redefining MBA Leadership Amid AI’s Rise with Human-Centric Skills
LIBA’s Rev. Dr. Arun: Redefining MBA Leadership Amid AI’s Rise with Human-Centric Skills CFOs Shift from Financial Stewards to Strategic Innovators in AI-Driven Economy
CFOs Shift from Financial Stewards to Strategic Innovators in AI-Driven Economy AI Revolutionizes Reverse Engineering: Legal Risks Demand Urgent Trade Secret Protections
AI Revolutionizes Reverse Engineering: Legal Risks Demand Urgent Trade Secret Protections