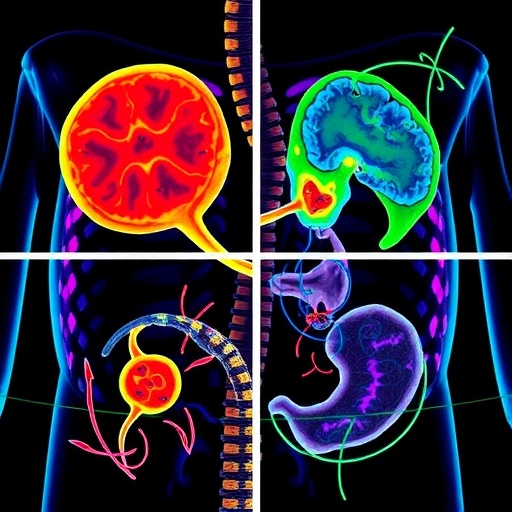
In a significant advancement for gastric cancer treatment, researchers led by Nguyen et al. have introduced innovative deep learning models aimed at enhancing risk stratification for patients diagnosed with this prevalent malignancy. Published in the Journal of Translational Medicine, the study demonstrates how digital pathology can be leveraged to analyze high-resolution images for predicting patient prognosis and responses to immunotherapy, addressing a critical need given gastric cancer’s substantial contribution to global mortality rates.
The research team evaluated an extensive dataset of thousands of digitized histopathological images, accurately categorized to reflect various stages of gastric cancer. Utilizing the principles of deep learning—a sophisticated subset of artificial intelligence—these models are designed to identify intricate differences in cellular structures that are often overlooked by conventional assessment methods. This capability enables the model not only to assess the malignancy of gastric tumors but also to predict their potential responsiveness to immunotherapeutic agents.
A notable aspect of the study is the application of transfer learning techniques, allowing the model to utilize knowledge from related datasets to adapt its predictions to the specific characteristics of gastric cancer tissue. The researchers developed a specialized architecture comprising convolutional neural networks tailored to explore histopathological features, such as immune cell density within the tumor microenvironment, which is crucial in determining immunotherapy outcomes.
To ensure the accuracy and reliability of their model, the researchers employed rigorous cross-validation techniques across multiple training and testing datasets. This approach mitigates the common issue of overfitting in machine learning models, yielding an impressive accuracy rate in predicting patient outcomes and indicating the model’s potential as a transformative tool in clinical settings.
Furthermore, the deep learning framework contributes significantly to the shift towards personalized medicine in oncology. By identifying which patients are more likely to benefit from immunotherapy, clinicians can make informed treatment decisions, optimizing therapeutic strategies. This is particularly vital given gastric cancer’s heterogeneous treatment responses, where some patients experience considerable tumor shrinkage while others show minimal or no improvement.
In their study, the authors emphasized the integration of clinical features with digital pathology inputs to enhance prediction accuracy. By correlating imaging data with clinical parameters—such as tumor stage, histological subtype, and patient demographics—they fortified the robustness of their deep learning model. This multi-dimensional approach not only elevates prognostic precision but also deepens the understanding of varying disease trajectories in gastric cancer.
Ethical considerations surrounding artificial intelligence in healthcare remain a contentious topic, yet the researchers advocate for transparency and interpretability in their model. They highlight the necessity for clinicians to comprehend the rationale behind specific predictions, fostering trust in AI-driven healthcare solutions. As such, methodologies were incorporated to elucidate the model’s predictions, enhancing its applicability in clinical environments.
With the field of digital pathology rapidly evolving, the authors call for ongoing research focused on standardizing imaging practices and data-sharing protocols. They urge collaborative efforts among global institutions to develop expansive databases, which will facilitate the creation of more comprehensive AI models representative of diverse populations.
The implications of this study extend beyond academic interest, as the healthcare community stands at the cusp of a new era where individualized patient profiles can significantly influence treatment pathways. This could not only improve survival rates in gastric cancer but also pave the way for broader applications of similar methodologies across various malignancies.
As healthcare professionals increasingly integrate insights generated from artificial intelligence, it is imperative that they receive training on the interpretation and application of these advanced analytical tools within their clinical practices. Such training will ensure a smooth transition to AI-enhanced therapeutic strategies, ultimately benefitting patients.
In summary, the pioneering work by Nguyen and colleagues underscores the transformative potential of deep learning models in revolutionizing prognostic assessments and therapeutic decisions for gastric cancer. As these technologies evolve, their promise for improving patient outcomes and personalizing treatment plans is significant. This research exemplifies the intersection of technology and medicine, setting the groundwork for future investigations that could lead to further advancements in the fight against cancer.
The pursuit of optimized patient care remains urgent as the healthcare sector endeavors to harness technological breakthroughs that can reshape oncology positively. Continued investment in the research and development of artificial intelligence applications will be crucial in paving the way for future innovations, aiming towards a future where cancer is not merely treated but effectively managed, if not eradicated.
See also Study Reveals Over 20% of YouTube’s New User Recommendations Are Low-Quality AI Content
Study Reveals Over 20% of YouTube’s New User Recommendations Are Low-Quality AI Content Bristol Myers Squibb Enhances Drug Development with Digital Technology for 34,000 Employees
Bristol Myers Squibb Enhances Drug Development with Digital Technology for 34,000 Employees CRISPR-GPT Powers AI-Enhanced Gene Editing as CASGEVY Therapy Gains Regulatory Approval
CRISPR-GPT Powers AI-Enhanced Gene Editing as CASGEVY Therapy Gains Regulatory Approval DoD Invests $1.3M in U of I’s AI Research to Enhance PTSD Diagnosis for Military Families
DoD Invests $1.3M in U of I’s AI Research to Enhance PTSD Diagnosis for Military Families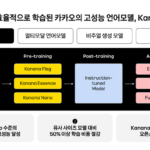 Kakao’s Kanana AI Model Achieves Higher Safety Ratings than Meta’s Mistral in First Evaluation
Kakao’s Kanana AI Model Achieves Higher Safety Ratings than Meta’s Mistral in First Evaluation