In a rapidly advancing technological landscape, the integration of artificial intelligence (AI) into critical sectors such as health care is gaining traction, despite ongoing concerns about its reliability. A bill introduced in the U.S. House of Representatives in early 2025 aims to permit AI systems to autonomously prescribe medications, prompting intense debate among health researchers and lawmakers regarding the feasibility and advisability of such measures. The implications of this legislation highlight the high stakes involved in AI deployment, especially when errors could lead to serious consequences, including patient fatalities.
Users often overlook AI’s shortcomings—such as misinterpreted speech, erroneous fact generation, or misguided navigation—because the technology can significantly enhance efficiency. However, as advocates push for minimal human oversight in high-stakes areas, the potential for errors raises critical questions about accountability and safety. Should AI systems fail in diagnosing or prescribing, it remains unclear who would be held responsible: pharmaceutical companies, software developers, or health care providers.
Research into complex systems reveals that AI’s inherent imperfections may stem from the very nature of its data. According to a study conducted by researchers, including those studying traffic light coordination and tax evasion detection, certain datasets may produce a baseline level of errors due to overlapping characteristics among categories. For instance, an AI model trained solely on age, weight, and height might distinguish between breeds like Chihuahuas and Great Danes but could struggle with similar-looking breeds like the Alaskan malamute and Doberman pinscher.
As Alan Turing, a pioneer in computer science, famously noted: “If a machine is expected to be infallible, it cannot also be intelligent.” This principle underlines a significant tension between the pursuit of intelligence through learning and the expectation of perfection. In a study published in July 2025, researchers found that efforts to classify complex datasets often yield less than ideal results. For instance, they attempted to predict which students would graduate on time from the Universidad Nacional Autónoma de México. Despite employing various AI algorithms, even the most effective reached only an 80% accuracy rate, indicating that substantial misclassification was unavoidable due to the similarities in students’ profiles.
The pursuit of more data to enhance AI accuracy can lead to diminishing returns, as substantial increases in dataset size may yield marginal improvements in predictive capabilities. For example, achieving just a 1% increase in accuracy may require 100 times more data, underscoring the challenges of improving AI models in meaningful ways. Additionally, unpredictable life events, such as job loss or personal crises, can further complicate the ability to accurately predict outcomes in a consistently changing environment.
Complexity emerges as a limiting factor in prediction accuracy, as the intricate interplay among the components of a system often results in unpredictable behavior. A car’s trajectory in city traffic exemplifies this notion; while speed can theoretically predict its future location, real-time interactions with other vehicles make precise predictions practically impossible beyond a short time frame.
This complexity also manifests in health care, where overlapping symptoms across different conditions can hinder accurate diagnoses. AI’s potential to misidentify patient needs could create legal ambiguities, especially in cases where misdiagnosis leads to harm. While humans also err, the stakes become particularly high with AI involvement, necessitating careful consideration of oversight in automated prescribing scenarios.
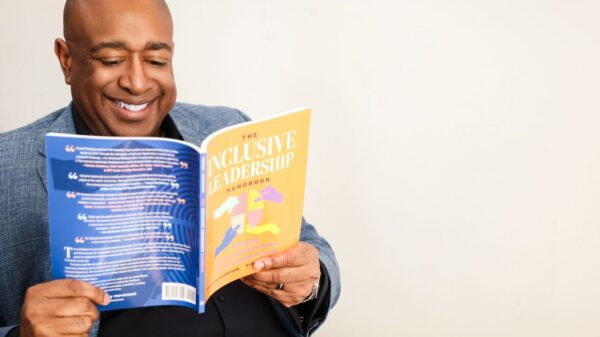
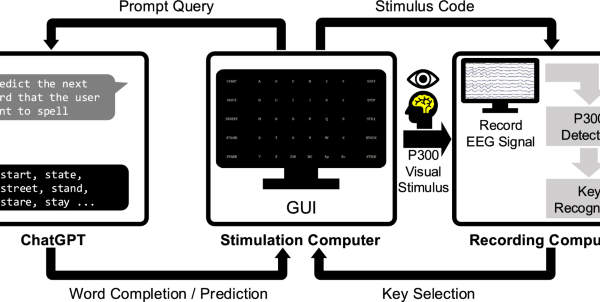
In many instances, a hybrid approach that combines human expertise with AI capabilities—referred to as “centaur” intelligence—may yield the best outcomes. For example, AI can assist physicians in identifying suitable drug therapies based on individual patient profiles. This collaborative model is already being explored within precision medicine initiatives.
Despite the potential benefits of AI in health care, prevailing common sense and caution advocate for human oversight in critical decision-making processes. The inherent imperfections of AI technology underscore the need for human involvement, especially when health and well-being are at stake. As society grapples with the implications of AI integration in health care, the call for a balanced approach—leveraging both human insight and technological advancements—will likely remain a topic of significant discussion.
See also UH Researchers Unveil AI Tool to Accurately Map Sun’s Magnetic Field in 3D
UH Researchers Unveil AI Tool to Accurately Map Sun’s Magnetic Field in 3D Lomonosov Team Achieves Multi-State Accuracy in Ultrafast Photodynamics with ML Potentials
Lomonosov Team Achieves Multi-State Accuracy in Ultrafast Photodynamics with ML Potentials Google Integrates Gemini AI into Search and Assistant, Enhancing User Experience with Smart Summaries
Google Integrates Gemini AI into Search and Assistant, Enhancing User Experience with Smart Summaries Kenya Achieves Historic UN Resolution on AI’s Environmental Sustainability at UNEA-7
Kenya Achieves Historic UN Resolution on AI’s Environmental Sustainability at UNEA-7 Purdue University Launches AI Working Competency Requirement for All Undergraduates
Purdue University Launches AI Working Competency Requirement for All Undergraduates