A recent study has unveiled a groundbreaking approach to understanding the costs associated with breast cancer surgery. Led by researcher He, J. and colleagues, the study employs ensemble machine learning techniques to predict surgical expenses and identify key factors driving these costs. This multifaceted strategy aims not only to enhance comprehension of financial implications but also to potentially transform surgical practices in oncology.
Breast cancer, one of the world’s most prevalent cancers, necessitates treatment strategies that balance clinical effectiveness with economic feasibility. As healthcare systems contend with rising expenses, grasping the financial landscape of surgical interventions becomes increasingly important. The research team’s use of advanced machine learning methods offers a potential template for future studies focused on optimizing cost-efficiency within medical practice. Their findings are expected to raise awareness and influence healthcare policies, ultimately aiming to improve patient care.
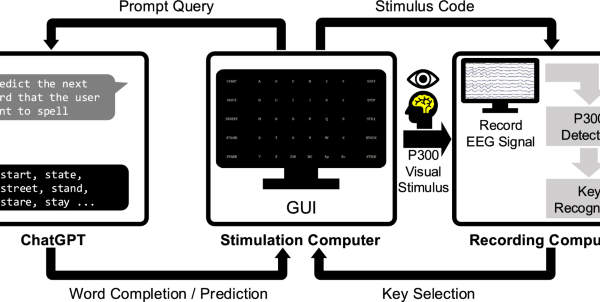
At the heart of the research is ensemble machine learning, which synergizes multiple algorithms to enhance predictive accuracy. Traditional models often depend on singular approaches, which can restrict the insights derived from data. In contrast, ensemble techniques leverage the strengths of various machine learning methods, thereby improving predictive performance and reliability. The approach exemplified by He and colleagues allows for thorough analysis of extensive datasets, establishing meaningful correlations between surgical costs and numerous influencing variables.
The data analyzed by the researchers encompasses a wide range of factors affecting surgical expenses, including patient demographics, treatment modalities, hospital characteristics, and post-operative care requirements. By examining these variables through ensemble machine learning, the team creates a detailed depiction of the economic landscape surrounding breast cancer surgery. This comprehensive view is essential for hospitals and healthcare providers striving to enhance operational efficiency while maintaining high-quality care for patients.
Beyond merely predicting costs, the research highlights the importance of understanding the factors influencing surgical expenses. Identifying unnecessary costs can lead to substantial savings for both healthcare systems and patients alike. The insights gleaned may inform policymakers in reforming reimbursement frameworks to better align financial incentives with optimal care practices. As hospitals adapt strategies based on this research, they may be better positioned to allocate resources effectively, targeting areas for cost savings without sacrificing patient care.
The machine learning framework utilized in this study also supports ongoing refinement of predictive models. As additional data becomes available, algorithms can be enhanced, leading to increasingly accurate predictions. This continuous improvement process mirrors advancements in technology across various sectors, heralding a transformative phase at the intersection of healthcare and data science. The adaptability of these machine learning solutions holds promise for the future of personalized medicine, equipping clinicians to make informed decisions based on both clinical evidence and economic realities.
For healthcare providers looking to harness the findings of this research, integrating machine learning models into current healthcare IT infrastructures is essential. Implementing these advanced models requires collaboration between data scientists and healthcare professionals to develop practical, user-friendly systems. Training staff to interpret and utilize these predictive tools is vital, as the ultimate objective is to translate data insights into actionable solutions that enhance patient outcomes and minimize costs.
However, the ethical implications surrounding the use of machine learning in healthcare cannot be overlooked. While the potential for accuracy and efficiency is substantial, it also raises concerns regarding data privacy and the risk of algorithmic bias. Researchers and practitioners must navigate these challenges carefully, fostering a culture of transparency and trust. Adhering to ethical guidelines in the deployment of machine learning models will be crucial to preserving the integrity of patient care and ensuring equitable advancements in the field.
As the healthcare industry increasingly embraces technological innovation, this study represents a significant step toward understanding the potential of machine learning in managing breast cancer treatment costs. By optimizing expenses and revealing key influencers, the research contributes to a growing body of literature that underscores the role of artificial intelligence in enhancing health service delivery. This work paves the way for more sustainable healthcare practices in the treatment of breast cancer.
The implications of this study are extensive, suggesting numerous avenues for further research. Future investigations could extend these findings to encompass other cancer types, different surgical procedures, or varied healthcare systems globally. The versatility of the ensemble machine learning approach positions it as a valuable asset for researchers seeking to uncover cost patterns and enhance surgical efficiency across diverse contexts.
As the medical community reflects on the insights offered by this study, the potential to reshape healthcare delivery comes into focus. Oncologists, hospital administrators, and policymakers alike stand to gain a clearer understanding of the financial dynamics associated with breast cancer surgery. Through targeted interventions informed by predictive analytics, the healthcare system can transition toward a model that prioritizes both patient care and fiscal responsibility, ensuring that individuals battling breast cancer receive necessary support without being overwhelmed by financial burdens.
This research signifies a promising frontier in breast cancer treatment, illustrating the transformative potential of data-driven solutions within medicine. The convergence of advanced technology with critical health challenges highlights the opportunities at hand for optimizing healthcare delivery. As the industry strives to embrace these advancements, it becomes evident that data-driven methodologies will increasingly shape the future of breast cancer treatment and healthcare as a whole.
See also Chandrakala Reveals Machine Learning Method for Acoustic Ball Bearing Fault Detection
Chandrakala Reveals Machine Learning Method for Acoustic Ball Bearing Fault Detection AI Expert John Sviokla: Adoption Accelerates as Companies Face Investment Risks
AI Expert John Sviokla: Adoption Accelerates as Companies Face Investment Risks AI Models Exhibit Bias Against Dialects, Reveals Study from Germany and the US
AI Models Exhibit Bias Against Dialects, Reveals Study from Germany and the US Researchers Expose Fault Injection Vulnerabilities in ML-Based Quantum Error Correction
Researchers Expose Fault Injection Vulnerabilities in ML-Based Quantum Error Correction AI Reveals Two New Subtypes of Multiple Sclerosis, Transforming Treatment Approaches
AI Reveals Two New Subtypes of Multiple Sclerosis, Transforming Treatment Approaches