In an era when the American healthcare system is grappling with significant challenges, personal stories like that of a recent patient highlight the ongoing issues of misdiagnosis and fragmented care. The patient, who faced a prolonged illness due to an overlooked diagnosis of mycoplasma pneumonia, spent a month navigating a healthcare labyrinth filled with blood tests, electrocardiograms, and numerous consultations before finally receiving the correct diagnosis. This experience was emblematic of a broader national crisis, as healthcare professionals are increasingly tasked with more responsibilities while coping with dwindling resources.
In March 2025, Secretary of Health and Human Services Robert F. Kennedy Jr. announced plans to reorganize the agency, vowing to do “more with less.” However, for many patients, this “less” translates to shorter appointments, fragmented care, and overwhelmed providers struggling under heavy caseloads. This trend is not an isolated incident; it reflects systemic issues exacerbated by reductions in healthcare funding, particularly during the previous administration, which has left many Americans facing serious risks of misdiagnosis.
Such misdiagnoses can have dire consequences. Take, for instance, the case of 6-year-old Daniel Witten, who was initially diagnosed with the flu but later hospitalized for serious complications related to a cavernous malformation. The situation dramatically changed when his mother took it upon herself to research potential treatments. Ultimately, she discovered a specialist capable of performing a life-saving surgery. This incident raises questions about the potential benefits of advanced technology, such as artificial intelligence, that could help in diagnosing conditions more accurately and quickly.
According to a July 2023 study published in the BMJ journals, approximately 371,000 people die annually in the U.S. due to misdiagnoses. This figure underscores the urgency of the situation, particularly in light of tragedies like that of college student Sam Terblanche, who died from sepsis after being discharged with a diagnosis of “acute viral syndrome.” The stark reality is that while the U.S. boasts the highest gross domestic product globally, it continues to resist adopting universal healthcare, unlike 72 other nations that have made such investments.
As of 2025, the average cost of a family health plan in the U.S. has soared to nearly $27,000, placing an enormous burden on families, particularly when the poverty line for a family of four is set at $32,150. The fragmentation and unaffordability of healthcare have become pressing issues, especially given the recent cuts to essential health insurance programs. While artificial intelligence is not a panacea, it may serve as one of the few scalable solutions remaining within a stretched-thin healthcare system.
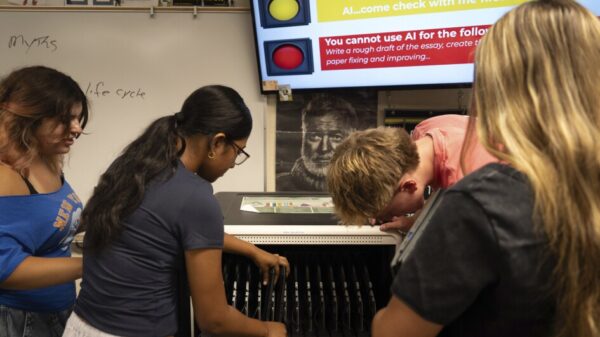
AI systems, trained on extensive clinical datasets, are showing promise in identifying overlooked conditions, recommending streamlined treatment plans, and prioritizing urgent cases. While current AI applications do not replace physicians, they offer valuable support that can act as a secondary layer of verification within a time-limited healthcare environment. This is particularly important as healthcare professionals face escalating demands on their time and expertise.
Nevertheless, the concerns surrounding AI in medicine are significant, encompassing issues like patient privacy, potential job displacement, and the accuracy of AI-driven diagnostics. However, it is crucial to understand that these challenges do not only affect healthcare providers; it is ordinary Americans who suffer from an expensive, rushed, and often dismissive healthcare system. If AI presents a viable and effective solution, stakeholders must engage with its development thoughtfully to ensure it improves rather than complicates the patient experience.
As the healthcare landscape evolves, the adoption of technology like AI could represent a critical turning point for American healthcare, potentially improving diagnostic accuracy and patient outcomes. The imperative now is for healthcare professionals and policymakers to embrace innovations that could alleviate the systemic issues plaguing the industry, ultimately benefiting those most affected by its shortcomings.
See also South Korea Downplays Impact of 25% US Tariff on AI Chips, Excludes Memory Products
South Korea Downplays Impact of 25% US Tariff on AI Chips, Excludes Memory Products Taiwan Invests $250B in U.S. Tech to Boost AI Chip Production Amid Trade Deal
Taiwan Invests $250B in U.S. Tech to Boost AI Chip Production Amid Trade Deal Alphabet Commits $93 Billion to Quantum Computing, Targets Industry Leadership
Alphabet Commits $93 Billion to Quantum Computing, Targets Industry Leadership Andrej Karpathy Challenges Nvidia’s Huang on AI’s Role in Coding and Productivity Gains
Andrej Karpathy Challenges Nvidia’s Huang on AI’s Role in Coding and Productivity Gains Anthropic Reveals AI’s Dependency on Human Input Quality in New Economic Index Report
Anthropic Reveals AI’s Dependency on Human Input Quality in New Economic Index Report