The health care industry is bracing for a critical debate over the payment structures for clinical artificial intelligence (AI) tools. As of the end of September, the Food and Drug Administration has authorized 1,357 AI-enabled medical devices, yet only a handful are being reimbursed by insurers. This disparity raises questions about the integration of AI in patient care.
Health policy experts, such as Ateev Mehrotra, chair of health services, policy, and practice at the Brown University School of Public Health, argue that the focus should shift from merely securing payments for individual technologies to leveraging AI to enhance clinician productivity and patient care efficiency. “If I could wave a magic wand, I would change our paradigm to: ‘How can we use AI to improve the productivity and efficiency of clinicians so that they can care for more patients at a high quality, at a lower cost?’” Mehrotra stated.
Conversely, industry stakeholders express concern that the lack of reimbursement will hinder the adoption of beneficial AI tools. The debate is expected to escalate in 2026, as more AI devices enter the marketplace. Currently, only three AI devices have garnered a permanent CPT code from the American Medical Association (AMA), a necessary step for securing payments from Medicare and most private insurers. The AMA has issued over 20 temporary category III codes to AI devices, many of which are anticipated to transition to permanent status.
In anticipation of a surge in AI technologies, the AMA is exploring the establishment of a new code category for AI, including tools requiring no physician input. Simultaneously, the Centers for Medicare and Medicaid Services is examining its payment models for AI, which have primarily been based on vendors’ assessments of their software. Legislative proposals aimed at formalizing payment pathways for AI have also surfaced.
The complexities of payment structures are already causing uncertainty within health systems. “Health systems are looking at AI and wondering how the heck they pay for this,” remarked Pelu Tran, CEO of AI governance company Ferrum Health.
Fee-for-Service Signals in Coronary Plaque Analysis
Starting in January, Medicare will implement a set national rate of just over $1,000 for AI technology analyzing coronary plaque in patients. This initiative represents one of the limited AI tools to receive a Category I CPT code, serving as a crucial benchmark as the AMA and CMS deliberate on broader payment strategies. Previous technology assessing blood flow through coronary arteries is also reimbursed at a similar rate, highlighting the slow evolution of AI payment frameworks.
“Payment for plaque analysis has been very spotty,” noted Eric Rubin, primary CPT adviser for the American College of Radiology. “It is slowly becoming more uniform, but we will have to see how this progresses over time.” The effective use of AI in this area will depend on physicians’ understanding of when to utilize the technology and how well they document patient conditions for reimbursement.
In the realm of breast imaging, many women opting for annual mammograms are now faced with AI add-ons designed to detect suspicious lesions. However, without insurer reimbursement, patients typically bear the cost, which ranges from $40 to $50 for such enhancements. Greg Sorensen, chief science officer at RadNet, emphasized that a self-pay model is not ideal, as it places the financial burden on patients rather than facilitating broader access through insurance coverage.
Despite these challenges, RadNet’s AI-based screening program has proven profitable, with approximately half of the 1.6 million annual mammograms opting for AI-enhanced services. Looking ahead, as out-of-pocket costs for these services continue to rise, there may be increasing pressure on insurers to adopt reimbursement models for AI applications in breast imaging.
In the absence of reimbursement structures, some health systems are choosing to invest in AI based on anticipated improvements in efficiency and health care quality. “If they judge based on the published literature or their own internal experience that this is adding enough value for them, then I think that we should use that as a sign,” Mehrotra remarked.
Several large academic medical centers are implementing opportunistic screening programs, employing existing radiological images to detect additional health risks. For example, NYU Langone is investigating the use of CT scans for signs of osteoporosis, while Emory Healthcare is developing algorithms to identify breast arterial calcification in standard mammograms. These initiatives present a potential triple win: improved patient outcomes, increased revenue for health systems, and cost savings for payers.
The outcomes of these AI applications and their financial implications will be closely monitored, contributing to the ongoing discourse around the integration of AI in health care. As the landscape evolves, striking the right balance between innovation and cost-effectiveness will be crucial for the sustained advancement of AI technologies in clinical settings.
For more information on the evolving landscape of AI in health care, visit the official sites of FDA, CMS, and AMA.
See also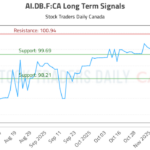 AI.DB.F:CA Trading Strategy Revealed—Buy at 99.69, Target 100.94 with Neutral Outlook
AI.DB.F:CA Trading Strategy Revealed—Buy at 99.69, Target 100.94 with Neutral Outlook Musk’s xAI Acquires Third Building, Boosting AI Compute Capacity to Nearly 2GW
Musk’s xAI Acquires Third Building, Boosting AI Compute Capacity to Nearly 2GW SoundHound AI Stock Plummets 56%: Assessing Buy Opportunities Amid Growth Potential
SoundHound AI Stock Plummets 56%: Assessing Buy Opportunities Amid Growth Potential 2026 Sees Surge in Power, Cooling, Networking Stocks as AI Dependency Grows
2026 Sees Surge in Power, Cooling, Networking Stocks as AI Dependency Grows OpenAI Launches Sora 2, Revolutionizing AI Image-to-Video Generation with Sound and Dialogue
OpenAI Launches Sora 2, Revolutionizing AI Image-to-Video Generation with Sound and Dialogue