A recent opinion study published in PLOS Digital Health challenges the prevailing notion that artificial intelligence (AI) operates as a non-human entity, warning that this mischaracterization obscures both its origins and associated risks. Titled “From Artificial to Organic: Rethinking the Roots of Intelligence for Digital Health,” the research posits that AI systems should be viewed as extensions of organic human intelligence shaped by human data, values, biases, and design choices. This conceptual shift, the authors argue, carries significant implications for accountability, safety, and governance in the healthcare sector.
The study traces the roots of AI thinking to the mid-20th century, where early pioneers conceptualized machine intelligence as a distinct, engineered phenomenon. Landmark milestones such as the Turing Test and the Dartmouth conference established the ambition to create intelligence separate from the human brain. Over the years, this perspective solidified into the idea that artificial intelligence could evolve into an autonomous cognitive force. However, the authors contend that contemporary AI systems present a different narrative.
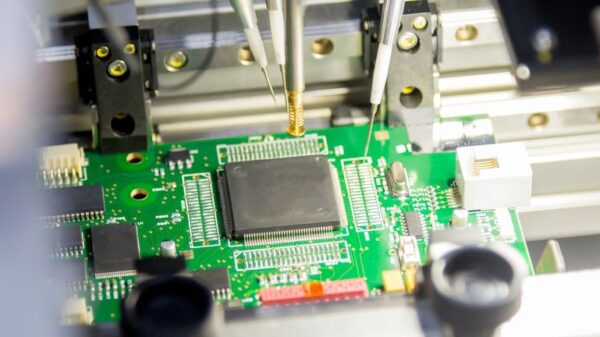
Current AI models, particularly those employed in healthcare settings, do not generate intelligence in isolation. They learn from vast amounts of human-generated data, including clinical records, medical images, scientific literature, and behavioral signals. Each output produced by these systems derives statistically from patterns embedded in human activities and knowledge, reinforcing the idea that AI intelligence is not entirely artificial or disconnected from its organic origins.
Neural networks, frequently cited as evidence of machine cognition, draw inspiration from biological brain structures. Their architecture, optimization, and evaluation are products of decades of neuroscience research translated into mathematical frameworks. Even the creativity and decision-making abilities of AI emerge from exposure to human language, medical reasoning, and clinical examples. Thus, the study reframes intelligence as a property characterized by organization and adaptability rather than by the material substrate on which it operates. Intelligence expressed through silicon circuits can still be fundamentally organic because it originates from human cognitive processes.
This distinction is crucial as it alters the framework for assigning responsibility. If AI systems mirror human inputs, then their errors, biases, and limitations cannot be dismissed as mere machine failures. Instead, they reflect amplified expressions of human choices encoded into data, algorithms, and objectives. The study emphasizes the need for a reevaluation of accountability, particularly in digital health, where AI systems play increasingly critical roles in high-stakes decisions like radiology triage and predictive analytics.
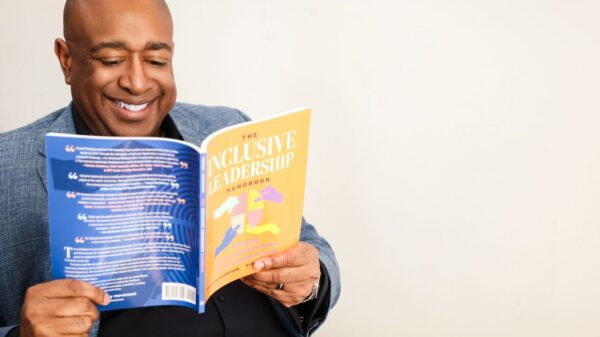
Understanding AI as organically rooted has direct implications for how these systems are evaluated and governed. Bias in medical AI cannot simply be brushed aside as a technical glitch; it mirrors biases present in clinical datasets, institutional practices, and historical healthcare inequities. If certain populations are underrepresented or misrepresented in training data, AI systems will reproduce those distortions at scale, leading to inequitable outcomes.
The authors assert that this reframing clarifies ethical responsibility among clinicians, developers, and institutions, as accountability remains for AI-driven outcomes. This challenges narratives that treat errors from AI as unpredictable or unavoidable consequences of autonomous systems. The paper also addresses the burgeoning interest in artificial general intelligence and superintelligence in healthcare, cautioning against equating scale with intelligence. While larger models can process more data more quickly, without careful organization and explainability, they risk exacerbating errors rather than enhancing care.
In clinical environments, speed must be harmonized with safety. The study underscores the necessity for uncertainty-aware systems capable of signaling when predictions are unreliable. Mechanisms for rollback and human intervention are also highlighted, as explainability is framed as a safety imperative, particularly when AI recommendations influence critical medical decisions.
Practical constraints such as data quality, variability across institutions, computational costs, and energy consumption further emphasize the need for designs inspired by biological efficiency rather than brute-force computational power. The researchers argue that the language used to describe AI profoundly shapes research priorities and regulatory approaches. The artificial versus natural divide often encourages a focus on scale and performance metrics, while an organic versus inorganic perspective emphasizes adaptability, integration, and shared responsibility.
This conceptual shift has profound implications for how AI systems are tested and regulated. Rather than relying on static benchmarks that assess accuracy on fixed datasets, the authors advocate for dynamic evaluation methods that gauge adaptability, calibration in changing conditions, and resilience to shifts in data distribution. This approach is particularly relevant in healthcare, where patient populations and clinical practices evolve continuously.
Furthermore, the organic framing encourages collaboration across diverse disciplines. Neuroscientists, clinicians, and AI engineers are urged to work together, treating intelligence as a continuum rather than a categorical divide. Such integration may lead to systems that align more closely with human cognition and clinical workflows, thereby reducing the risks associated with unsafe automation.
Accountability mechanisms also emerge as a central focus. The study calls for governance structures embedded within AI systems, rather than added as afterthoughts. This includes architectural features that log changes, track model evolution, and trigger abstention when confidence is low, ensuring AI behavior is transparent and auditable, in line with medical and legal standards of responsibility.
As discussions of superintelligence gain traction in policy and industry circles, the authors urge caution, suggesting that intelligence should not be defined solely by performance metrics or autonomy. In the realm of healthcare, intelligence must be measured by its capacity to support human judgment, ensure safety, and uphold ethical boundaries, paving the way for a future where AI enhances, rather than compromises, patient care.
See also AI inside Inc. Stock Falls 4.37% to JPY 2582; Future Forecasts Signal Mixed Outlook
AI inside Inc. Stock Falls 4.37% to JPY 2582; Future Forecasts Signal Mixed Outlook NVIDIA GPUs Drive AI Boom as Data Center Sales Surge, Stock Hits New Highs
NVIDIA GPUs Drive AI Boom as Data Center Sales Surge, Stock Hits New Highs Bernie Sanders Calls for AI Moratorium, Warns of Economic Impact on American Workers
Bernie Sanders Calls for AI Moratorium, Warns of Economic Impact on American Workers Broadcom Hits $352.13 as AI Demand Soars, Yet Margins Face Pressure Ahead of Q1
Broadcom Hits $352.13 as AI Demand Soars, Yet Margins Face Pressure Ahead of Q1