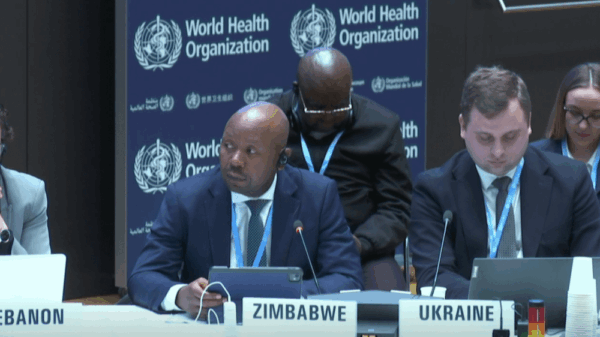
A significant debate over the governance of artificial intelligence (AI) and digital health emerged at the World Health Organization (WHO) Executive Board meeting on Wednesday, as low and middle-income countries raised concerns over data ownership and equity in healthcare. The discussions took place during the Board’s 156th session in Geneva, Switzerland, which runs from February 3 to 11, 2025.
Countries warned that the rapid deployment of AI technologies could exacerbate health inequalities without robust governance frameworks. They cautioned that without sustainable financing and equitable guardrails, the integration of AI into health systems could endanger “data sovereignty.” The debate was largely shaped by a WHO report that outlined a digital transformation strategy spanning from 2028 to 2033, highlighting the need for reliable, representative data to avoid amplifying existing biases and inefficiencies.
“Innovation alone is not enough,” stated Hans Kluge, WHO Regional Director for Europe. He emphasized that digital tools could widen existing gaps in healthcare if not paired with the necessary skills, governance, and trust. Kluge also warned of the potential for a new digital divide, which could further disadvantage vulnerable populations.
To address these challenges, the WHO has initiated a tripartite collaboration with the International Telecommunication Union and the World Intellectual Property Organization to refine its digital strategy. In addition to the discussions on AI governance, the board also decided to advance consultations aimed at strengthening the global health workforce code, while tackling the problem of substandard medicines through a new operational framework.
The meeting highlighted a regulatory rift concerning AI, with high-income regions like the European Union and the United States moving to establish guiding principles while low and middle-income countries (LMICs) emphasize ownership and ethical governance. The European Medicines Agency (EMA) and the U.S. Food and Drug Administration (FDA) have made strides in the regulatory landscape, but a formal global standard remains elusive.
During the session, the European Union, represented by Bulgaria, underscored the importance of harmonizing health data and information systems, asserting that they form the “essential foundation” for AI applications. In support, Israel proposed the creation of “regulatory sandboxes” to enable safe testing of new technologies while balancing economic considerations.
In contrast, the African Region, represented by Cameroon, redirected the focus from technical standards to ownership issues, advocating for rigorous ethical governance. The representative expressed concerns that multinational corporations might exploit health data from the Global South to train AI models and develop products for profit.
Barbados further reinforced this sentiment, asserting that health data should be treated as a “national asset” and should remain under local control, rejecting donor-funded surveys that do not address long-term sustainability. The country positioned itself as a “living laboratory” for digital innovation, advocating for sustainable financing models to support universal health coverage.
The board also confronted the escalating crisis of health worker migration, with Zimbabwe issuing a strong call for wealthier nations to co-invest in the education and retention of healthcare professionals from countries with fragile health systems. The issue of targeted recruitment from these nations has led to a significant “brain drain” to the Global North.
Pakistan echoed Zimbabwe’s call for co-investment but highlighted the lack of binding commitments from high-income countries. The United Kingdom, a major destination for healthcare talent, acknowledged the need for clearer guidance on ethical recruitment practices while maintaining that the Global Code of Practice is fundamental.
The WHO board also addressed the critical issue of substandard and falsified medical products, which delegates deemed a significant threat to public health. Since 2013, WHO’s surveillance system has identified over 10,000 suspect products, with a recent spike in contaminated cough syrups raising alarms about public safety.
Togo, representing the African Region, described the proliferation of substandard medicines as a “scourge” exacerbated by informal markets and open borders. The region called for innovative financing to bolster regulatory authorities in vulnerable settings. Ukraine highlighted the threats posed by unregulated online sales, urging the WHO to help secure supply chains for high-risk pharmaceuticals.
To address these pressing issues, the Board noted an urgent need for market surveillance technologies, including the Epione reporting tool, to track suspect products in real-time. As the WHO prepares to draft a global strategy for the next five years, the outcomes of these discussions will be pivotal for shaping future health governance and ensuring equitable access to healthcare innovations.
See also Palantir’s AI Platform Fuels 1,700% Stock Surge, Unlocks $4.3B in New Contracts
Palantir’s AI Platform Fuels 1,700% Stock Surge, Unlocks $4.3B in New Contracts Germany”s National Team Prepares for World Cup Qualifiers with Disco Atmosphere
Germany”s National Team Prepares for World Cup Qualifiers with Disco Atmosphere 95% of AI Projects Fail in Companies According to MIT
95% of AI Projects Fail in Companies According to MIT AI in Food & Beverages Market to Surge from $11.08B to $263.80B by 2032
AI in Food & Beverages Market to Surge from $11.08B to $263.80B by 2032 Satya Nadella Supports OpenAI’s $100B Revenue Goal, Highlights AI Funding Needs
Satya Nadella Supports OpenAI’s $100B Revenue Goal, Highlights AI Funding Needs